Original Article
October 2020, 28:1
First online: 24 November 2020
Original Article
Graft Patency Rate and Risk Factors for Graft Failure among Symptomatic Post Coronary Artery Bypass Graft Surgery Patients
See Woan Shiang,1 Simon Jerome Vendargon,1 Syed Rasul Bin Ghouse Syed Hamid,1 Benjamin Leo Cheang Leng,2 Law Kian Boon3
1 Cardiothoracic Surgery Unit, Hospital Sultanah Aminah Johor Baru, Johor, Malaysia
2 Cardiology Unit, Hospital Sultanah Aminah Johor Baru, Johor, Malaysia
3 Institute For Clinical Research, National Institute Of Health, Ministry Of Health, Malaysia
Correspondence: Dr See Woan Shiang
E mail: seewoanshiang@gmail.com
Contact number: +60177320924
Fax number: +6076878580
ABSTRACT
BACKGROUND
Malaysia, a multiracial country, has been burdened by ischemic heart disease, the leading cause of death for the past 10 years. The success of coronary artery bypass grafting surgery (CABG) particularly depends on the continued patency of aortocoronary grafts. The study aims to identify the graft patency rate and risk factors of graft failure among symptomatic post CABG patients.
METHODS
Data were collected from 80 patients with a history of CABG, who underwent conventional coronary angiography for refractory angina in Hospital Sultanah Aminah Johor, Malaysia from January 2014 till December 2018. The graft patency was evaluated with conventional coronary angiography. Graft patency was assessed with the Kaplan-Meier method. Differences between graft patency were tested with log-rank test at a 5% significance level and result with p-value <0.05 was considered statistically significant.
RESULTS
Among the 80 post CABG patients with cardiac symptoms, there were 2 patients with acute myocardial infarction (2.5%) and 24 patients with NSTEMI (30%). 22 patients (27.5%) were found to have all grafts patent despite being persistently symptomatic. Left internal mammary arterial (LIMA) graft remained as the best conduit with a significantly better short, medium, and long term patency (up to 20 years) compared to SVG graft (Log-rank test, p-value < 0.05). Indian race and age less than 70 years had higher risk of SVG graft stenosis.
CONCLUSION
Type of conduits remains the most important factor in determining the coronary artery bypass graft patency, with LIMA produces the best patency rate in both short and long term.
INTRODUCTION
Ischemic heart disease (IHD) is the leading cause of death for the past 10 years from 2005 to 2019 in Malaysia, mainly for population aged 15 to 64 years old.1 The surgical intervention for coronary artery disease is mainly by coronary artery bypass grafting surgery (CABG), which is the operation most commonly performed in cardiac surgery. CABG has been shown to effectively improve survival and symptoms among patients with severe multiple coronary artery disease.2, 3 The success of coronary revascularization particularly depends on the continued patency of aortocoronary grafts, which include left internal mammary artery (LIMA) and saphenous vein grafts (SVGs).4, 5
Graft failure is associated with poorer outcomes. It is defined as graft whose patency is threatened by a hemodynamically significant lesion, or ≥ 75% stenosis, in the inflow tract, outflow tract, or within the body of the graft.6 It can be divided into three temporal categories: early (zero to 30 days), midterm (30 days to one year) or late (after one year).6, 7 Early graft failure occurs in up to 15% of patients after coronary artery bypass grafting surgery. it is mainly caused by the thrombotic events within the anastomosis site. A fully developed plaque will require three to five years to form on a new graft.6, 8
Therefore, even with graft revascularization after surgery, patients with coronary artery disease remain at high risk for recurrent acute coronary disease. Salvage of the failed grafts is an important clinical challenge to both the surgeons and cardiologists. Thus, more researches have now focused on methods to monitor and control the development of graft failure. By understanding the pathophysiology of graft stenosis, multiple factors including operative techniques, underlying disease and follow up therapy, are important to successful management of graft failure.7, 8, 9
OBJECTIVES
Identify the graft patency rate and risk factors of graft failure among symptomatic post CABG patients. STUDY DESIGN AND METHOD
This is a cross-sectional study conducted in Hospital Sultanah Aminah Johor, Malaysia. All symptomatic patients with prior CABG who proceeded with coronary angiography in Hospital Sultanah Aminah from January 2014 till December 2018 were included in the study. Patients’ angiographic findings, pre-CABG cardiac status, and CABG operative findings were retrospectively reviewed and compared. The patients’ clinical outcomes were further compared by the presence of LIMA graft which was known to affect long term survival of CABG patients. The study was approved by the National Medical Research Register Malaysia. The primary endpoint for this study is graft patency over time by graft type and territory among these symptomatic patients with a history of CABG in Hospital Sultanah Aminah Johor, Malaysia. Graft failure is defined as one of a patent graft whose patency is threatened by a hemodynamically significant lesion, or ≥ 75% stenosis, in the inflow tract, outflow tract, or within the body of the graft, usually by coronary angiography. Coronary angiography is the gold standard for coronary artery disease diagnosis.10 It is performed by a cardiologist to assess the patency of coronary arteries and grafts post CABG. In case multiple coronary angiographies were performed post CABG to assess graft failure, the last coronary angiography findings were included in the study. Duration of graft patency is calculated from the day of CABG until the day of last coronary angiography post CABG, measured in months.
STATISTICAL ANALYSIS
Analysis were performed using R version 3.6.1. Descriptive analysis was done for socio-demographic variables at baseline. Numerical data such as age were summarised using mean ± standard deviation (sd) or median. Categorical data such as ethnicity and graft stenosis were summarised using rate in percentages (%). Difference between continuous variables were compared using independent t-test at 5% significance level. Associations between categorical data were tested using Pearson’s chi-square test. Conduit patency curve were estimated using the Kaplan-Meier method and difference groups were tested using the log-rank test. Risk factors association to graft stenosis was assessed by simple cox regression. A value of p<0.05 (two-sided) was considered statistically significant.
RESULTS
From January 2014 to December 2018, there was a total of 80 (70 men, 10 women) post CABG patients with cardiac symptoms proceed for coronary angiography. There were two patients with acute myocardial infarction (2.5%), 24 patients with Non ST-elevated Myocardial Infarction (NSTEMI) (30%), 25 patients with unstable angina (31.3%), and 29 patients with stable angina (36.3%). Two post CABG patients were excluded from the study due to acute myocardial infarction and asystole prior to coronary angiography. The baseline demographic characteristics were shown in Table 1.

GRAFT FAILURE
Out of these 80 patients, Coronary angiography revealed at least one graft was occluded among 57 patients (72.3%). 23 patients (27.7%) were found to have all grafts remain patent despite persistently symptomatic. Based on the coronary angiographic findings, the patients were advised for medical therapy or second revascularizations including Percutaneous Coronary Intervention (PCI) or redo-CABG. The therapeutic management was decided following treating cardiologist and cardiac surgeon’s discussion. There were nine PCI (11.3%), five redo-CABG (6.3%), and 66 medical treatment (82.5%) for these symptomatic patients.
PRESENCE OF LIMA
The patients were further divided based on the presence of LIMA grafts. Coronary angiography revealed that graft occlusion was found in eight patients (72.7%) in the non-LIMA group (n= 11). 49 patients (71.0%) with LIMA anastomoses had at least one graft occluded. Presence of LIMA was not protective against graft occlusion. The mean interval from CABG operation to the postoperative angiographic assessment of these 80 patients was 107.06 months (8.9 years), with duration range from the shortest at seven months to the longest at 267 months (22.2 years). The mean interval from CABG operation to coronary angiography study was longer among patients with LIMA graft (111.7 months), but the difference was not statistically significant. (table 2 and table 3)

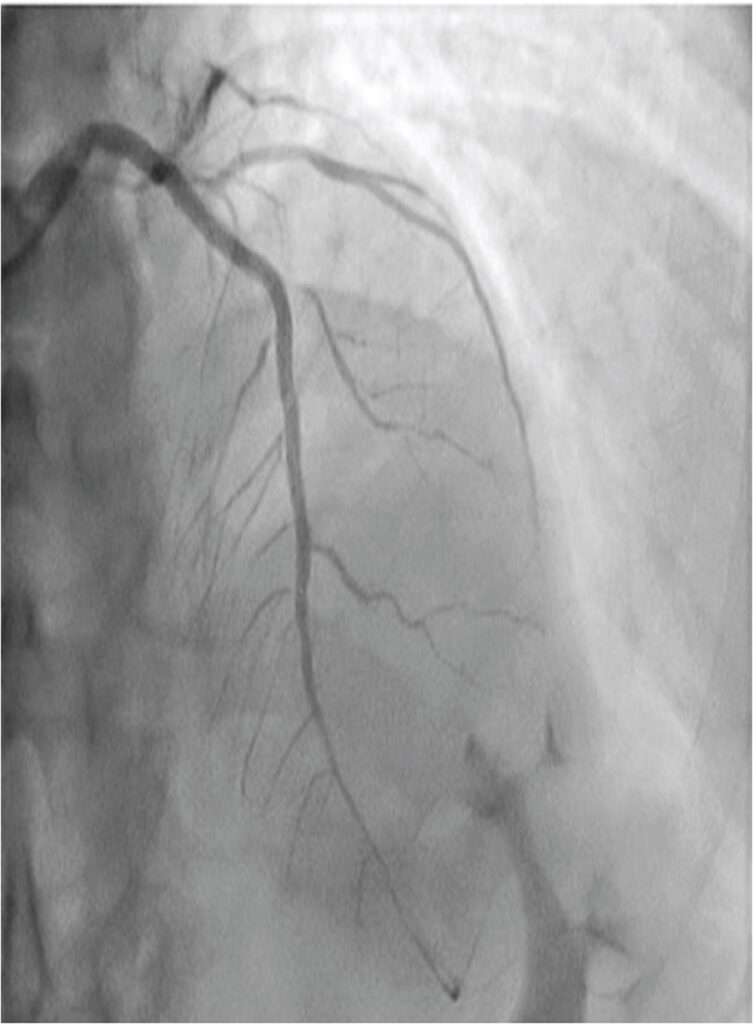
GRAFT PATENCY RATE- THE TYPE OF GRAFTS
There was a total of 239 grafts, which divided into 69 LIMA, five radial artery, and 165 SVG grafts. Based on the coronary angiography, we found that LIMA graft had significantly better short, medium, and long term patencies compared with SVG graft (Log-rank test, p-value < 0.05). (Table 4, Figure 1) Radial artery graft patency was not included for comparison due to its small number (n=5) to generate statistical value.


Figure 1
Graft patency curve for comparison of SVGs and LIMA grafts over time (months)
SVGS GRAFT PATENCY RATE- DISTAL ANASTOMOSIS SITE
Overall, there was a total of 93 SVG graft stenosis (56.3%, N= 165). SVG patencies were further compared based on its distal anastomosis site either left anterior, left posterior or right territory. No significant difference of graft patency over time based on the distal anastomotic site. (Table 5, Figure 2)RISK FACTOR ASSOCIATIONS WITH SVGS GRAFT PATENCY
Among 80 these post CABG patients, 57 patients (72.3%) had at least one graft occluded. Out of 69 LIMA grafts, eight grafts were occluded upon coronary assessment, compared to 93 graft occlusions of 165 SVG grafts. The associations between preoperative risk factors and SVG graft occlusion were examined with simple cox regression, as shown in Table 6. Age and race were found to be associated with increased risk of SVG graft occlusion. Age less than 70 years had higher risk of graft stenosis compared to age above 70 years (HR 2.64, CI 1.40 – 4.99, p = .002). Indian race was associated with significant increased risk of graft occlusion compared to other races (HR 2.30, CI 1.14 – 4.67, p = .021).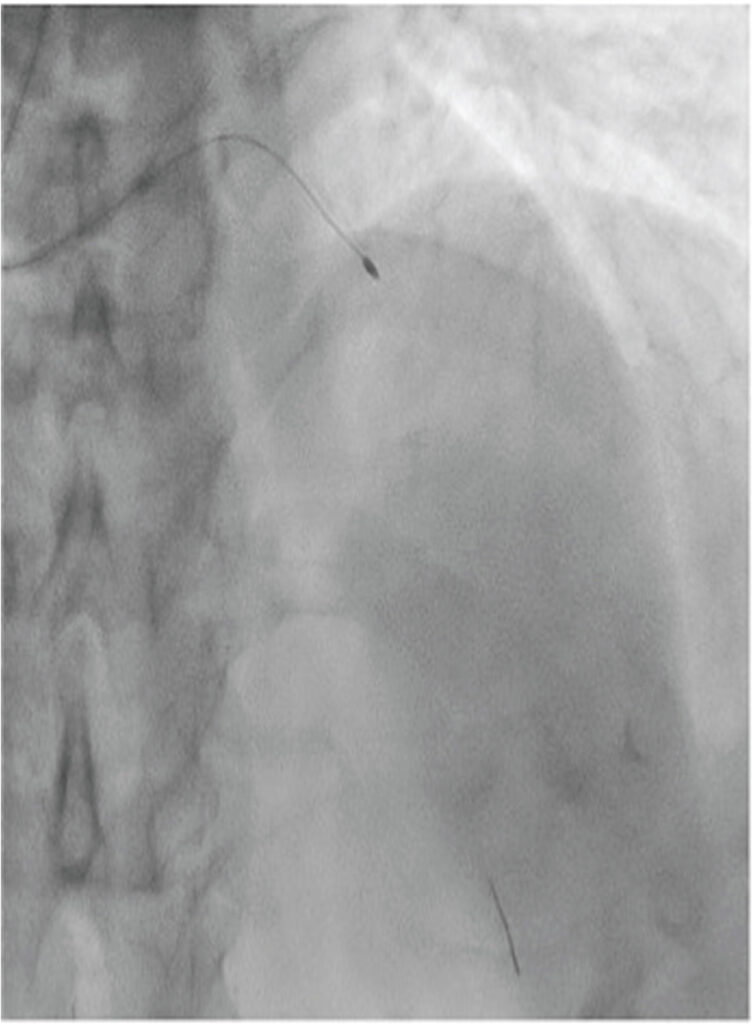
Figure 2
Graft patency curve for comparison of SVGs based on the distal anastomosis site – left anterior (LAD/ D1), left posterior (OM/LCX/ INT) and right territory (RCA/PDA/ PLV)
DISCUSSION
In comparison to medical treatment and PCI, CABG surgery undoubtedly reduces angina severity and frequency in at least 80- 85% of patients. Though coronary artery bypass surgery has stood the test of time, its success mainly depends on the long term patency of the grafts.
Recurrent limiting angina after CABG, however, has been a major challenge to the treating surgeon and physician. To patients, it is much more grievous than mortality. In our center, there were a total of 80 patients present with refractory angina after CABG surgery from 2014 till 2019. Despite optimal medical management, the other option is revascularization, either PCI or redo surgery. Redo- CABG is often fraught by patients due to its high mortality risk, 2-3 times higher than the first surgery with relatively less promising angina alleviation. Redo- CABG is associated with greater risk of bleeding, exploration difficulty due to adhesions, and potential injury to the existing grafts. Therefore, redo- CABG is only limited to selected good candidates.[11] High-risk patients are often left with medical treatment. In our center, there is 6.3% of a redo- CABG among the 80 patients with recurrent symptoms, in comparison to 82.5% of medical treatment. It is inadequate in most of the cases, and this is when interventional cardiologists these days could offer endo-coronary techniques as alternative solutions.
For decades, refractory angina after CABG surgery is often associated with graft failure. A prospective study from Reda AA et al in 2014 showed 56% of grafts were occluded among post CABG patients with recurrent angina.12 In our center, up to 72.8%, post-CABG patients of refractory angina were found to have at least one graft occluded. By retrospective evaluation, the graft failure rate was not affected by the presence of LIMA (71% versus 72.7%, p ≤0.609). Interestingly, the duration from CABG to coronary angiography assessment among symptomatic patients with LIMA was 33.9 months longer than patients with total venous grafts. However, we failed to prove it statistically due to the relatively small sample size which represents the main limitation of our study. The protective impact of IMA grafting on survival has been well established. Cameron A and colleagues found that IMA grafting reduced the risk of dying by a factor of 0.73, and was a significant predictor of late survival.13 Our study suggested, despite survival, LIMA is important in the delay of recurrent symptoms presentation. Further local studies with larger sample sizes are required for investigation.
Among symptomatic post CABG patients, 27.7% of patients had all grafts remain patent. Their coronary angiographic findings were associated with the progression of native coronary vessels as the culprits of their refractory angina. Progressive native coronary atherosclerosis beyond the grafted segments or previously non grafted vessels often results in more fibrotic and calcified occlusion. It is challenging to tackle the lesion through usual balloon angioplasty, and cutting balloon angioplasty followed by stenting is often required. PCI of a native coronary artery is technically more preferable than PCI to the SVG of the same territory, as SVG PCI carries a higher acute and longterm risk.[11, 14] Theoretically, SVG intervention causes dislodge of atheroembolic debris, and through contrast flow, it is flushed to smaller caliber distal coronary vessels, results in periprocedural angina and ischaemic myocardial infarction.
Out of the 239 conduits, Kaplan-Meier graft patency curves showed that LIMA appeared to have a statistically significant better graft patency at five, ten, and twenty years. In a comparison of extended late graft patency follow up at 20 years, SVGs graft patency was drastically reduced to 6.7%, as compared to 62.7% of LIMA graft. It showed that LIMA graft has prognostic benefits for early, mid, and long term patency compared to SVGs. It is consistent with large trial analysis Veterans Affairs trial which showed the 10-year patency was 61% for SVGs and 85% for LIMA grafts.15
The hypothesis is during the first year post CABG, platelet aggregation, growth factor secretion, endothelial dysfunction, inflammation, luminal foam cell accumulation, decreased local fibrinolytic potential from plasminogen activator inhibitor-1 upregulation and marked intimal hyperplasia result in up to 15% of SVG grafts occluded.1 Subsequently, lipid deposition within intimal hyperplasia and atherosclerotic plaque formed. After 6 years, neointimal growth, atherosclerosis, and vein graft arterialization causes narrowed lumen and increased pressure load. This process accelerates the graft occlusion rate and at 11 years only 50-60% of the grafts will be patent. At 10 years, only up to 40% of the patent venous grafts will be free of disease. Arterial grafts especially the left internal mammary artery, on the other hand, offer a patency rate of over 90% at 10 years when anastomosed to the left anterior descending coronary artery.15
Undoubtedly, LIMA to LAD territory produced the best graft patency over time. But there was no apparent graft-by-territory interaction when SVG graft patency rate was compared based on the distal anastomotic sites. Overall, SVGs had a mean graft patency rate of 88.6%, 59.3%, and 6.7% at five, ten, and twenty years. The finding was, in contrast, to study by Sabik JF et al. The study in 2011 concluded that bypass grafts performed to the left anterior descending coronary artery produce the best patency, followed by those performed to diagonals, circumflex branches, and the posterior descending artery which have intermediate patency; and those performed to the main right coronary artery have the worst patency.17
Graft stenosis was associated with multiple risk factors. Besides surgical related risk factors. It is highly related to smoking status, hyperlipidemia and diabetes mellitus.8 In our study, the implication of preoperative comordities on graft failure was not significant due to the small sample size. Age less than 70 years was associated with higher risk of graft occlusion. Interestingly, Indian race was twice the risk of SVG graft occlusion compared to Chinese and Malay race in Malaysia. The finding was consistent with a review article by Volgman AS et al in 2018 which stated that Indians have higher proportional mortality rates from atherosclerotic cardiovascular disease compared with other Asian groups.21 Further large scale prospective studies are needed to compare the graft stenosis among different age groups and race groups in Malaysia.
LIMITATION
The major limitation of the study is the single center with retrospective data collection and a relatively small number of patients. Additionally, other confounding factors including medication compliance, preoperative coronary disease severity, intraoperative factors like conduits and anastomosis quality, cross-clamp time, and perioperative morbidities were not assessed in the study.18, 19, 20 The radial arterial graft was not included in the graft analysis due to its small number to generate statistical value (five from a total of 240 grafts), which may lead to the underestimation of its net clinical benefit. However, since the universal sampling of all symptomatic patients from a singlecenter was used in the study and patients’ records were followed for up to 20 years, we believe that a meaningful conclusion may be drawn from our data.
CONCLUSION
In Hospital Sultanah Aminah, Johor, the majority (72.3%) of post CABG patients with refractory angina who had coronary angiography, have graft failure. However, up to 28.7% of symptomatic post CABG patients are found to have all grafts patent with progression of native coronary arterial disease. Indian race and age less than 70 years were associated with higher risk of SVG graft stenosis.We support the use of LIMA graft to LAD territory as it produces a statistically significant better five, ten, and twenty years patency compared to SVG graft, with a patency rate of 98.4%, 90.6%, and 62.7% respectively. Meanwhile, we find no difference in graft-by-territory interaction when SVG grafts are used.
KEYWORDS
Graft Patency, Coronary artery bypass graft surgery, Left internal mammary artery, Refractory angina, Saphenous vein graft
ACKNOWLEDGMENTS
We acknowledge the Director General of Ministry of Malaysia who approved this manuscript to publish in journal.
REFERENCES
1. Department of Statistics Malaysia, Official Portal. Statistics on causes of death, Malaysia, 2019.
2. Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, et al, 2011 ACCF/AHA Guideline for coronary artery bypass graft surgery, Circulation 124:2610-2642, 2011. CrossRef Pubmed
3. Yusuf S, Zucker D, Peduzzi P, Fisher LD, Takaro T, Kennedy JW, et al, Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration, Lancet 344:563–570, 1994. CrossRef Pubmed
4. Yamane Y, Uchida N, Okubo S, Impact of the size mismatch between saphenous vein graft and coronary artery on graft patency, Gen Thorac Cardiovasc Surg 65: 25–31, 2017. CrossRef Pubmed
5. Hess CN, Lopes RD, Gibson CM, Hager R, Wojdyla DM, Englum BR, et al, Saphenous vein graft failure after coronary artery bypass surgery: insights from PREVENT IV, Circulation 130:1445–1451, 2014. CrossRef Pubmed
6. Lopes RD, Mehta RH, Hafley GE, Williams JB, Mack MJ, Peterson ED, et al, Project of Ex Vivo Vein Graft Engineering via Transfection IV (PREVENT IV) Investigators. Relationship between vein graft failure and subsequent clinical outcomes after coronary artery bypass surgery, Circulation 125:749–756, 2012. CrossRef Pubmed
7. Beijk MA, Harskamp RE, Treatment of coronary artery bypass graft failure. In: Aronow WS (ed) Artery bypass, InTech 193–237, 2013.
8. Gao J, Liu Y, Li YM, Review of risk factors, treatment, and prevention of saphenous vein graft disease after coronary artery bypass grafting, J Int Med Res 46(12):4907-4919, Dec 2018. CrossRef Pubmed
9. Inaba Y, Yamazaki M, Ohono M, Yamashita K, Izumida H, Hayashi K, et al, No-touch saphenous vein graft harvesting technique for coronary artery bypass grafting, Gen Thorac Cardiovasc Surg 68(3):248-253, Mar 2020. CrossRef Pubmed
10. Nadeem A, Angiographic study of coronary grafts, Pakistan Armed Forces Medical Journal 68(Suppl-1), S202-05, 2018.
11. Shahabuddin S, Ansari JA, Siddiqui FJ, Amanullah M, Sami SA, Redo coronary artery surgery; early and intermediate outcomes from a tertiary care hospital in a developing country, J Pak Med Assoc 61:31-35, 2011. Pubmed
12. Reda AA, Abdel Azeez WF, Ahmad MK, Samy NI, Management of coronary insufficiency after coronary artery bypass graft surgery, Menoufia Med J 27:570, 2014. CrossRef
13. Cameron A, Green GE, Kemp HG, Role of internal mammary artery in reoperation for coronary artery disease, Adv Cardiol 36:84–9, 1988. CrossRef
14. Yin L, Xiujun Z, Hua J, Mingdong G, Lin W, Yutian S, et al, Percutaneous coronary intervention strategies and prognosis for graft lesions following coronary artery bypass grafting, Exp Ther Med 9(5):1656–1664, May 2015. CrossRef Pubmed
15. Veteran Administration Coronary artery Bypass Surgery Co operative Study Group, Eleven-year survival in the Veterans Administration randomized trial of coronary bypass surgery for stable angina, N. Engl. J Med 311:1333- 1339, 1984. CrossRef Pubmed
16. Yayla, C, Canpolat, U, Akyel, A, Association between platelet to lymphocyte ratio and saphenous vein graft disease, Angiology 67:133– 188, 2016. CrossRef Pubmed
17. Sabik JF III,Understanding saphenous vein graft patency, Circulation 124(3):273-275, 2011. CrossRef Pubmed
18. Sher-i-Murtaza M, Baig MA, Raheel HM, Early outcome of Coronary Artery Bypass Graft Surgery in patients with significant Left Main Stem stenosis at a tertiary cardiac care center, Pak J Med Sci 31(4):909–914, 2015. CrossRef Pubmed
19. Khan JK, Shahabuddin S, Khan S, Bano G, Hashmi S, Sami SA, Coronary artery bypass grafting in South Asian patients: Impact of gender, Ann Med Surg (Lond) 2;9:33-7, Jun 2016. CrossRef Pubmed
20. Kim, YH, Oh, HC, Choi, JW, No-touch saphenous vein harvesting may improve further the patency of saphenous vein composite grafts: early outcomes and 1-year angiographic results, Ann Thorac Surg 103:1489– 1497, 2017. CrossRef Pubmed
21. Volgman AS, Palaniappan LS, Aggarwal NT, Gupta M, Khandelwal A, et al, Atherosclerotic cardiovascular disease: in South Asians in the United States: Epidemiology, Risk factors, and treatments. A Statement from the American Heart Association, Circulation 138(1): e1-e34, 2018.
Copyright Information
